Co-Morbid Conditions
What Other Disorders Usually Accompany ADHD?
According to Dr. Flick, there are numerous psychological and medical conditions that are often associated with ADHD. These may often share symptoms with ADHD or may involve ADHD-like behaviors.
Associated Medical Conditions
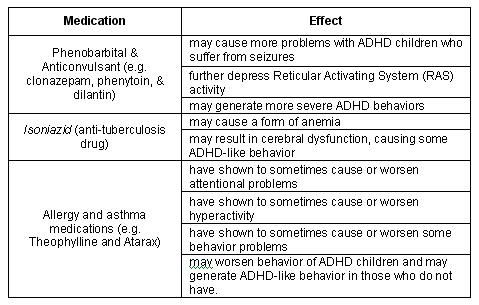
Reaction to Some Drugs and Medications
There are drugs for numerous medical conditions that can cause ADHD-like behavior, impairment of attention, increased motor activity, or impulsivity to individuals without ADHD. On the other hand, these medications may exacerbate the behavior in children with ADHD. Some drugs that seem to have these effects are tabulated below.
Tourette’s Syndrome
This is characterized by sudden, involuntary, and recurrent specific movements and vocalizations. These “tic” movements typically include grunting, hissing, barking, whistling, sniffing, snorting, and clearing of the throat. ADHD appears to 50% of individuals with Tourette’s.
Narcolepsy
This disorder overrules the right-brain function of vigilance or wakefulness. It is characterized by sleep attacks and rapid eye movement at inappropriate times during the day, which is different from sleepy state that is often observed in ADHD children.
Anemia
Anemia or the decrease in the number of circulating red blood cells includes symptoms of dizziness, drowsiness, headache, and awakening problems. According to Dr. Flick, studies have associated anemia with “personality disturbance, conduct problems, feelings of inadequacy, and immaturity.”
Fragile-X Syndrome
This is a chromosomal disorder which is the second most common cause of mental retargdation with mostly males being affected. Some symptoms of Fagile-X include impairments of interest, attention, and behavior. However, its association with ADHD can not still be generalized because only four cases were studied.
Movement Disorders
Movement disorder just like the characteristics of Sydenham’s Chorea, especially when accompanied by irritability and obsessive compulsive symptoms, could be confused with symptoms of ADHD.
Thyroid Dysfunction
Symptoms of hyperthyroidism like tremor, increased nervousness (overactivity), sweating, and rapid heart beat could also be mistaken for ADHD.
Sleep Apnea
Sleep apnea (SA) causes insufficient oxygenation of the blood and shows symptoms of loud snoring, pauses in respiration during sleep, daytime hypersomnolence, weight gain, disturbed sleep, and deficits in attention, motor efficiency, and psychomotor ability. Dr. Flick noted Findley’s report that problems in concentration, complex problem solving, and short-term recall are also symptoms of SA.
Sinusitis
Sinus infections affect airflow through the nasal passages and may generate the same symptoms as sleep apnea. Decreased alertness manifested by poor attention and overactivity may also be expected.
Head Injury
Head trauma or injury due to external force may produce a weakened or altered state of consciousness. Head injured children and adolescents display attention problems and hyperactivity, aside from other cognitive skills and intellectual performance.
Associated Psychological Conditions
As noted by Dr. Flick, 1/3 to ½ of teens with ADHD will have additional behavioral/emotional problems. Other psychological disorders may have many symptoms that mimic ADHD behavior. These may appear independent or co-morbid with ADHD.
Adjustment Disorders
Adjustment disorder, or the growth of clinically significant emotional or behavioral symptoms as a reaction to a particular psychosocial stressor or stressors, may be taken into account when ADHD children experience significant stress in the classroom.
Anxiety
About ¼ of teens with ADHD experience anxiety. There are two co-morbid conditions of anxiety that are sometimes associated with ADHD. These are the Generalized Anxiety Disorder and the Post-Traumatic Stress Disorder (PTSD). Generalized Anxiety Disorder includes symptoms of impairment in one’s attention and concentration, and errors of misjudgment in one’s responding. While PTSD, or the delayed painful response to an unusual and severely upsetting event, features depression, anxiety, disturbance of conduct, withdrawal, and interference with one’s personal life, work, or academic adjustment.
As noted by Dr. Flick, ADHD and anxiety appear to be at the opposite ends of arousal continuum. It is very seldom for them to co-exist and when they do, it is found more often in the predominantly inattentive type of ADHD. What’s interesting about the two is their difference in somatic (?) reactions to states of emergency. Anxiety shows overarousal and confusion and ADHD displays optimal arousal state, calmness and a more effective reaction.
Depression/Dysthymia
Depressive thoughts cause interference with thinking and sustained attention. Sleep difficulties and motoric restlessness similar to the symptoms of ADHD is also present in individuals with depression/dysthymia. Flick noted that 25% to 30% of ADHD adolescents may experience serious depression. The symptoms manifested include sadness, loss of pleasure, negative views of self, hopelessness, poor concentration and memory, confusion, changes in appetite and sleep, fatigue, increase in aches and pain, passivity, and indifference in activities.
Bipolar Disorders
Bipolar disorder of Manic Depression occurs when an individual experience depressive episodes and manic episodes alternately and swiftly, with only a brief return to normality in between. Hypomanic episodes, just like ADHD, show excessive activity, impulsivity, poor judgment, and denial of problems. ADHD is distinguishable through its early age of onset, its chronic rather than episodic pattern, and the lack of abnormally extensive and elevated mood. Intensified behavior problems with violent temper outbursts occur when ADHD and Manic Depression co-exists in an individual.
Mental Retardation
A child is considered to have Mental Retardation (MR) when his intellectual functioning/quotient (IQ) is 70 or below. This, together with mood disorder, pervasive developmental disorder, stereotypic movement disorder, and ADHD are associated with each other due to a general medical condition like head trauma.
Learning Disabilities
Attention plays an important role in learning. However it is insufficient enough especially if the cortical ability of the brain to process information is impaired just like the case of an individual who has LD. These learning problems are associated with the mental ability of a child in academic areas such as reading, math, spelling, handwriting, and language development. LD children may exhibit ADHD-like behaviors such as excessive motor activity and poor attention skills due to frustrations. Similarly, ADHD children may have LD because of their difficulty in focusing and sustaining attention.
Conduct Disorder (CD) and Oppositional Deficit Disorder (ODD)
In clinical settings, as noted by Dr. Flick, at least 2/3 of patients with ADHD also has oppositional deficit disorder (ODD) and conduct disorder (CD). When this co-morbid CD has an “early onset” (prior to age 10), individuals may manifest antisocial behaviors throughout their lifespan. In a “late onset” condition, on the other hand, the problem does not last as long and as pervasive as the first group and has a possibility that it will not continue past adolescence. Children and adolescents with this co-morbid condition are more likely to display more physical aggression to both people and animals, destruction of property, theft, violation of rules, driving problems, anti-social behavior, and drug abuse.
On the other hand, ODD displays a milder form of chronic behavior problems. This is the most frequent occurring co-morbid disorder with roughly 40% to 65% of those with ADHD. This is manifested by stubborn negativism, hostile and defiant behaviors, but without serious violation of the rights of others.
Obsessive Compulsive Disorder (OCD)
This disorder, according to Dr. Flick, is characterized by excessively persistent and disturbing thoughts with ritualistic behavior, mental activity, and irresistible motor behaviors. These characteristics affect one’s focus and attention. OCD may be more frequently associated with the predominantly inattentive type of ADHD.
According to Dr. Flick, there are numerous psychological and medical conditions that are often associated with ADHD. These may often share symptoms with ADHD or may involve ADHD-like behaviors.
Associated Medical Conditions
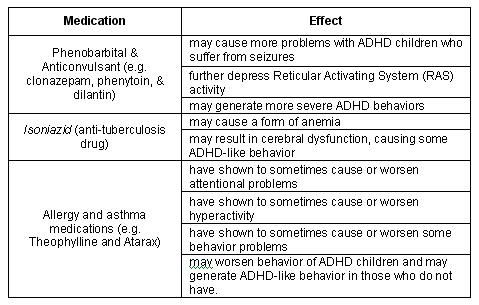
Reaction to Some Drugs and Medications
There are drugs for numerous medical conditions that can cause ADHD-like behavior, impairment of attention, increased motor activity, or impulsivity to individuals without ADHD. On the other hand, these medications may exacerbate the behavior in children with ADHD. Some drugs that seem to have these effects are tabulated below.
Tourette’s Syndrome
This is characterized by sudden, involuntary, and recurrent specific movements and vocalizations. These “tic” movements typically include grunting, hissing, barking, whistling, sniffing, snorting, and clearing of the throat. ADHD appears to 50% of individuals with Tourette’s.
Narcolepsy
This disorder overrules the right-brain function of vigilance or wakefulness. It is characterized by sleep attacks and rapid eye movement at inappropriate times during the day, which is different from sleepy state that is often observed in ADHD children.
Anemia
Anemia or the decrease in the number of circulating red blood cells includes symptoms of dizziness, drowsiness, headache, and awakening problems. According to Dr. Flick, studies have associated anemia with “personality disturbance, conduct problems, feelings of inadequacy, and immaturity.”
Fragile-X Syndrome
This is a chromosomal disorder which is the second most common cause of mental retargdation with mostly males being affected. Some symptoms of Fagile-X include impairments of interest, attention, and behavior. However, its association with ADHD can not still be generalized because only four cases were studied.
Movement Disorders
Movement disorder just like the characteristics of Sydenham’s Chorea, especially when accompanied by irritability and obsessive compulsive symptoms, could be confused with symptoms of ADHD.
Thyroid Dysfunction
Symptoms of hyperthyroidism like tremor, increased nervousness (overactivity), sweating, and rapid heart beat could also be mistaken for ADHD.
Sleep Apnea
Sleep apnea (SA) causes insufficient oxygenation of the blood and shows symptoms of loud snoring, pauses in respiration during sleep, daytime hypersomnolence, weight gain, disturbed sleep, and deficits in attention, motor efficiency, and psychomotor ability. Dr. Flick noted Findley’s report that problems in concentration, complex problem solving, and short-term recall are also symptoms of SA.
Sinusitis
Sinus infections affect airflow through the nasal passages and may generate the same symptoms as sleep apnea. Decreased alertness manifested by poor attention and overactivity may also be expected.
Head Injury
Head trauma or injury due to external force may produce a weakened or altered state of consciousness. Head injured children and adolescents display attention problems and hyperactivity, aside from other cognitive skills and intellectual performance.
Associated Psychological Conditions
As noted by Dr. Flick, 1/3 to ½ of teens with ADHD will have additional behavioral/emotional problems. Other psychological disorders may have many symptoms that mimic ADHD behavior. These may appear independent or co-morbid with ADHD.
Adjustment Disorders
Adjustment disorder, or the growth of clinically significant emotional or behavioral symptoms as a reaction to a particular psychosocial stressor or stressors, may be taken into account when ADHD children experience significant stress in the classroom.
Anxiety
About ¼ of teens with ADHD experience anxiety. There are two co-morbid conditions of anxiety that are sometimes associated with ADHD. These are the Generalized Anxiety Disorder and the Post-Traumatic Stress Disorder (PTSD). Generalized Anxiety Disorder includes symptoms of impairment in one’s attention and concentration, and errors of misjudgment in one’s responding. While PTSD, or the delayed painful response to an unusual and severely upsetting event, features depression, anxiety, disturbance of conduct, withdrawal, and interference with one’s personal life, work, or academic adjustment.
As noted by Dr. Flick, ADHD and anxiety appear to be at the opposite ends of arousal continuum. It is very seldom for them to co-exist and when they do, it is found more often in the predominantly inattentive type of ADHD. What’s interesting about the two is their difference in somatic (?) reactions to states of emergency. Anxiety shows overarousal and confusion and ADHD displays optimal arousal state, calmness and a more effective reaction.
Depression/Dysthymia
Depressive thoughts cause interference with thinking and sustained attention. Sleep difficulties and motoric restlessness similar to the symptoms of ADHD is also present in individuals with depression/dysthymia. Flick noted that 25% to 30% of ADHD adolescents may experience serious depression. The symptoms manifested include sadness, loss of pleasure, negative views of self, hopelessness, poor concentration and memory, confusion, changes in appetite and sleep, fatigue, increase in aches and pain, passivity, and indifference in activities.
Bipolar Disorders
Bipolar disorder of Manic Depression occurs when an individual experience depressive episodes and manic episodes alternately and swiftly, with only a brief return to normality in between. Hypomanic episodes, just like ADHD, show excessive activity, impulsivity, poor judgment, and denial of problems. ADHD is distinguishable through its early age of onset, its chronic rather than episodic pattern, and the lack of abnormally extensive and elevated mood. Intensified behavior problems with violent temper outbursts occur when ADHD and Manic Depression co-exists in an individual.
Mental Retardation
A child is considered to have Mental Retardation (MR) when his intellectual functioning/quotient (IQ) is 70 or below. This, together with mood disorder, pervasive developmental disorder, stereotypic movement disorder, and ADHD are associated with each other due to a general medical condition like head trauma.
Learning Disabilities
Attention plays an important role in learning. However it is insufficient enough especially if the cortical ability of the brain to process information is impaired just like the case of an individual who has LD. These learning problems are associated with the mental ability of a child in academic areas such as reading, math, spelling, handwriting, and language development. LD children may exhibit ADHD-like behaviors such as excessive motor activity and poor attention skills due to frustrations. Similarly, ADHD children may have LD because of their difficulty in focusing and sustaining attention.
Conduct Disorder (CD) and Oppositional Deficit Disorder (ODD)
In clinical settings, as noted by Dr. Flick, at least 2/3 of patients with ADHD also has oppositional deficit disorder (ODD) and conduct disorder (CD). When this co-morbid CD has an “early onset” (prior to age 10), individuals may manifest antisocial behaviors throughout their lifespan. In a “late onset” condition, on the other hand, the problem does not last as long and as pervasive as the first group and has a possibility that it will not continue past adolescence. Children and adolescents with this co-morbid condition are more likely to display more physical aggression to both people and animals, destruction of property, theft, violation of rules, driving problems, anti-social behavior, and drug abuse.
On the other hand, ODD displays a milder form of chronic behavior problems. This is the most frequent occurring co-morbid disorder with roughly 40% to 65% of those with ADHD. This is manifested by stubborn negativism, hostile and defiant behaviors, but without serious violation of the rights of others.
Obsessive Compulsive Disorder (OCD)
This disorder, according to Dr. Flick, is characterized by excessively persistent and disturbing thoughts with ritualistic behavior, mental activity, and irresistible motor behaviors. These characteristics affect one’s focus and attention. OCD may be more frequently associated with the predominantly inattentive type of ADHD.


<< Home